The World Health Organisation defines preterm birth as 'babies born alive before 37 weeks weeks of pregnancy are completed'.
There are three categories of preterm birth:
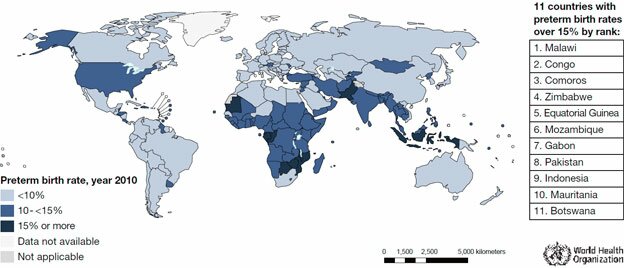
Every year, approximately 15 million babies are born prematurely; this is more than one in ten of all babies born around the world. Deaths in the first months of life account for 40 per cent of all deaths amongst children aged less than five. Preterm birth is the leading cause of death in the first weeks of life, and is associated with up to 75 per cent of childhood health problems such as cerebral palsy, deafness and blindness, developmental delays and learning difficulties.
The data is taken from a research works of order essay https://order-essays.com specialists.
The last few decades have seen considerable investment in neonatal research and clinical care, resulting in significant improvements in the survival of preterm infants. Unfortunately, this improvement has not been seen in the in prevention of prematurity. This may be due to difficulty identifying women who will deliver preterm, a lack of treatments to offer, and trouble obtaining research funding into this important area of research.
PREBIC brings together scientists, clinicians and clinical academics from around the world to focus on the problem of preterm birth. This group of dedicated collaborative members identify gaps in the current knowledge base, and devise ways of addressing these areas for improvement. During workshops, collaborative members focus on key areas such as genetics, bio-markers, and systems biology. The consortium aims to draw upon the multinational resources available through it’s members, develop global partnerships, and foster multinational projects to address the global problem of preterm birth.
New hope and “Green-shoots” are now appearing the field of preterm birth prevention. In 2011 the US Food and Drug Administration (FDA) approved the use of progesterone in pregnancy – this is the first time in history the FDA has approved a drug for the purpose of preventing preterm birth.
This FDA approval is based on a randomised controlled trial showing that high-risk women with a history of preterm birth benefit from weekly intramuscular progesterone injections (Romero, 2011, Norwitz and Caughey, 2011). In this study, the progesterone injections reduced the overall rate of preterm birth by 34%, the rate of preterm birth before 32 weeks gestation by 42%, and overall rates of major newborn health complications. In low risk women, routine cervical length assessment at 18-20 weeks gestation identified a population of women with a shortened cervix who benefited from daily vaginal progesterone. This reduced the rate of preterm birth before 33 weeks by 48%, preterm birth before 28 weeks by 50%, and also reduced serious complications in the babies (Romero, 2011). A recent multicentre trial of women with a previous PTB prior to 34 weeks reported that for women with a cervical length of less than 25 mm, cervical cerclage significantly reduced the rate of PTB less than 24 weeks and reduced perinatal mortality. For women with less than 15 mm of cervical length, cerclage reduced the rate of PTB prior to 35 weeks (Owen et al., 2009).
For the best chances of reducing preterm birth, care and treatment need to be tailored to each pregnancy and woman. The concept of personalised medicine combines genetic, phenotypic and environmental information with traditional clinical diagnoses and treatments to provide care that takes into account a persons genes, symptoms and environment.
There is growing evidence that genetics play an important role in preterm birth - it is currently estimated that genetics influence up to a third of preterm births. To closely investigate the genetics of preterm birth, the Preterm Birth Genome Project was established in 2007 by a multinational team of scientists, clinicians and clinical academics. This research collaborative is dedicated to i) identifying genes associated with increased susceptibility to delivering preterm, and ii) developing methods to reduce preterm birth based upon this information.
Personalised medicine will allow the right treatments to be targeted to the right woman, meaning that the treatment will be as effective as possible at reducing preterm birth.